Introduction
Diabetes is a chronic condition that significantly impacts the lives of millions of people worldwide, affecting their overall health and quality of life. This complex disease primarily revolves around the body’s ability to manage blood sugar (glucose), which serves as a critical energy source for our cells. Maintaining blood glucose levels within a healthy range is essential for the proper functioning of various bodily systems. When these levels become disrupted, the consequences can lead to severe health complications that threaten not only physical well-being but also emotional stability and daily functioning.The regulation of glucose is primarily governed by insulin, a hormone produced by the pancreas. In individuals diagnosed with diabetes, the body faces two main challenges: it either produces an inadequate amount of insulin or becomes resistant to the insulin that is produced, resulting in elevated blood glucose levels. Prolonged exposure to high blood sugar can lead to extensive damage to multiple organs and systems, increasing the risk of serious complications such as cardiovascular diseases, kidney failure, retinopathy (eye problems), and neuropathy (nerve damage).The significance of understanding diabetes cannot be overstated, as it is not merely a singular condition but encompasses various forms, including Type 1 diabetes, Type 2 diabetes, and gestational diabetes. Each type has its unique characteristics, causes, and symptoms of diabetes. Recognizing the symptoms of diabetes associated with each type is essential for early diagnosis and intervention, which can significantly enhance the prognosis and overall quality of life for affected individuals. This article aims to delve deeply into the symptoms of diabetes related to each type, providing a comprehensive understanding of what to look for to ensure timely medical attention and effective management strategies. By shedding light on these symptoms of diabetes, individuals can take proactive steps toward monitoring their health, fostering a greater awareness of their bodies, and seeking the necessary support when needed.
Understanding diabetes
Diabetes can be categorized into three primary types: Type 1 Diabetes, Type 2 Diabetes, and Gestational Diabetes. Each type is characterized by unique underlying causes, risk factors, and symptoms of diabetes that differentiate them from one another. Type 1 Diabetes is primarily an autoimmune condition in which the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells located in the pancreas. This process leaves individuals with Type 1 diabetes unable to produce insulin, which is essential for glucose regulation. As a result, they find themselves dependent on external insulin therapy for survival. This type of diabetes typically manifests in children and young adults but can occur at any age. The symptoms of Type 1 diabetes often present abruptly and can be quite severe. They include excessive thirst, frequent urination, extreme fatigue, and rapid weight loss. The sudden onset of these symptoms can be alarming, and the rapid progression of the disease necessitates immediate medical intervention to prevent serious health complications.
Conversely, Type 2 Diabetes arises when the body develops resistance to insulin or fails to produce sufficient insulin to maintain normal glucose levels. This form of diabetes is more prevalent and has a significant correlation with lifestyle factors such as poor dietary habits, physical inactivity, and obesity. The symptoms of diabetes associated with Type 2 diabetes tend to develop gradually, often over several years, making early diagnosis challenging and increasing the risk of severe complications that can impact health over time. Many individuals may remain undiagnosed for years, inadvertently exposing themselves to risks that could be mitigated through early intervention.
Gestational Diabetes is another form that occurs exclusively during pregnancy when the body is unable to produce enough insulin to meet the increased demands of both the mother and the developing fetus. Although gestational diabetes typically resolves after childbirth, it significantly raises the mother’s risk of developing Type 2 diabetes later in life. Moreover, it poses risks to the unborn child, including excessive birth weight and complications during delivery. Understanding the distinct characteristics and symptoms of diabetes associated with each type is crucial for early recognition and intervention. This knowledge can prevent long-term health complications, enhance well-being, and lead to better health outcomes for individuals at risk or already diagnosed with the condition.

Genraly symptoms of diabetes
The general symptoms of diabetes are closely linked to elevated blood glucose levels, which can significantly affect bodily functions and overall health. One of the most common symptoms of diabetes is frequent urination (polyuria). When blood sugar levels rise beyond a certain threshold, the kidneys work overtime to filter out the excess glucose by producing more urine. This process can lead to dehydration, prompting another prevalent symptom: increased thirst (polydipsia). Individuals may find themselves experiencing an overwhelming and persistent thirst as their bodies strive to replenish the fluids lost through frequent urination. This cycle of excessive urination and thirst can be exhausting, leaving individuals feeling fatigued and uncomfortable.
Additionally, unexplained weight loss is a notable symptom, particularly in Type 1 diabetes. Even with normal or increased food intake, individuals may lose weight because their bodies cannot effectively utilize glucose for energy. This inefficiency leads the body to break down fat and muscle for fuel, resulting in noticeable and often alarming weight loss within a short timeframe. Weight loss can be particularly distressing, as it is often accompanied by feelings of anxiety and frustration. Alongside these primary symptoms of diabetes, extreme hunger (polyphagia) may manifest as well. Despite eating adequate amounts of food, the body continuously signals for more energy due to its inability to properly utilize glucose. This sensation can become overwhelming, leading individuals to overeat in an attempt to satisfy their hunger, which paradoxically can contribute to weight gain, especially in Type 2 diabetes.
Beyond these primary symptoms of diabetes, individuals with diabetes frequently experience fatigue, a persistent feeling of exhaustion that does not improve with rest. This fatigue is rooted in the body’s cells not receiving the necessary energy from glucose, even when blood glucose levels are high. When insulin is deficient or the body becomes resistant to its effects, glucose cannot enter the cells, leading to feelings of weakness and lethargy. The experience of fatigue can significantly hinder daily activities, making it difficult to concentrate, engage in social interactions, or perform physical tasks. Furthermore, blurred vision is another common symptom linked to elevated blood sugar levels. High glucose levels can cause fluid to be pulled from the lenses of the eyes, resulting in swelling and distorted shapes, making it challenging to focus clearly. This symptom may fluctuate throughout the day and can become more pronounced after meals. If blood sugar levels remain uncontrolled for an extended period, individuals face an increased risk of developing diabetic retinopathy, which can lead to serious eye conditions, including vision loss.
Additionally, individuals may notice that cuts or wounds take longer to heal than usual. The slow healing of wounds is attributed to high glucose levels, which disrupt the body’s natural healing processes by diminishing blood flow and impairing the function of white blood cells, essential for fighting infections and repairing tissues. This slow healing can be particularly concerning for individuals with diabetes, as untreated injuries, especially on the feet, may go unnoticed and lead to severe infections or ulcers that could necessitate amputation.

Tingling, Pain, or Numbness in Hands and Feet
One of the more severe complications associated with long-term diabetes is diabetic neuropathy, a condition characterized by nerve damage resulting from consistently high blood sugar levels. This form of nerve damage primarily affects the peripheral nerves, which are responsible for transmitting signals from the brain and spinal cord to the rest of the body, including the hands, feet, and legs. As diabetes progresses, individuals may begin to experience tingling, pain, or numbness in these areas. The sensations can vary significantly, ranging from mild discomfort to severe pain that interferes with daily activities, often worsening at night when blood flow to the extremities may decrease. The onset of diabetic neuropathy is typically gradual, beginning with minor discomfort and advancing to debilitating pain. Many individuals describe the discomfort as a burning sensation, sharp pain, or an uncomfortable feeling of pins and needles.
For some, this pain can become unbearable, making it difficult to perform simple tasks such as walking or standing for extended periods. The discomfort may also lead to sleep disturbances, as individuals struggle to find comfortable positions that alleviate the pain. Over time, prolonged high glucose levels can inflict damage on these nerves, leading to additional symptoms of diabetes, including loss of sensation. This loss of sensation can pose significant risks, as untreated injuries, especially on the feet, may go unnoticed, potentially resulting in severe infections or ulcers that require medical intervention. Diabetic neuropathy is a progressive condition, meaning it worsens over time if blood sugar levels are not effectively managed.
The potential for serious complications stemming from diabetic neuropathy cannot be understated. For instance, individuals with reduced sensation in their feet may not feel the pressure of shoes or the pain of a blister, allowing these minor injuries to worsen unchecked. Regular foot inspections, proper footwear, and foot hygiene are crucial components of diabetes management to prevent complications stemming from neuropathy. Additionally, routine check-ups with healthcare providers can help monitor nerve function and implement early intervention strategies. Individuals experiencing these symptoms of diabetes should consult healthcare professionals for early intervention and management strategies to preserve nerve function and prevent further damage.
Skin Problems
Individuals with diabetes are particularly susceptible to a variety of skin problems, primarily due to the effects of elevated blood sugar levels on both the immune system and blood circulation. One common issue is dry and itchy skin, which arises when the body loses fluids due to frequent urination, leading to dehydration. This loss of moisture can result in dry, flaky skin that may become uncomfortable and irritating. The presence of dry skin can also lead to scratching, increasing the risk of cuts and infections. Additionally, high glucose levels compromise the skin’s ability to heal and fend off infections, making individuals more prone to skin irritations, rashes,
and fungal infections.
The yeast infection is another common skin problem among individuals with diabetes, particularly in warm, moist areas of the body, such as under the breasts, armpits, and between the toes. The high sugar levels in the blood and urine provide an ideal environment for yeast to thrive, leading to infections that can cause discomfort, redness, and itching. Furthermore, people with diabetes may also experience boils, which are painful lumps that form under the skin due to bacterial infections. These boils can develop on any part of the body, particularly in areas that experience friction or moisture. Eruptive Xanthomatosis is a lesser-known skin condition associated with uncontrolled diabetes, characterized by small, firm yellowish bumps that appear on the skin, particularly on the back of the arms, buttocks, and thighs. These bumps are a result of fat accumulation in the skin due to elevated blood sugar levels.
Effective management of diabetes is crucial to preventing these skin problems. Keeping blood sugar levels within the recommended range can significantly reduce the likelihood of skin complications and promote overall skin health. Individuals should practice good hygiene, moisturize regularly, and pay attention to any skin changes, seeking medical advice promptly if they notice unusual symptoms.
Increased Risk of Infections
Another critical aspect of diabetes is its association with an increased risk of infections. Elevated blood glucose levels impair the immune system’s ability to function optimally, reducing the body’s defenses against infections. Individuals with diabetes are particularly susceptible to urinary tract infections (UTIs), skin infections, and respiratory infections due to the impact of high glucose levels on the immune response. UTIs, in particular, are prevalent among women with diabetes, often stemming from elevated blood sugar levels that promote bacterial growth in the urinary tract.
Skin infections, such as boils and fungal infections, are also common in individuals with diabetes, primarily due to the high glucose levels providing a conducive environment for bacteria and fungi to thrive. Furthermore, individuals may experience recurring infections, which can be both frustrating and alarming, particularly if left untreated. The persistent cycle of infections can lead to a decline in overall health and well-being.
Moreover, an elevated risk of gum disease and oral infections is another concerning aspect of diabetes. High blood sugar levels can lead to inflammation and a weakened immune response in the gums, making individuals more vulnerable to gum infections and complications such as tooth decay. Routine dental care, including regular check-ups and good oral hygiene practices, becomes essential for individuals with diabetes to mitigate the risk of oral infections.
Recognizing the symptoms of diabetes associated with increased infection risk is crucial for prompt intervention and treatment. Individuals experiencing recurrent infections should seek medical attention to evaluate their blood sugar levels and overall health status.
Summary Table of Common Symptoms of Diabetes
| Symptom | Description |
|---|---|
| Frequent urination (polyuria) | Increased urination leading to dehydration and excessive thirst. |
| Increased thirst (polydipsia) | Persistent thirst due to fluid loss from frequent urination. |
| Unexplained weight loss | Loss of weight despite normal or increased food intake due to ineffective glucose utilization. |
| Extreme hunger (polyphagia) | Continuous sensation of hunger even after eating due to insufficient glucose uptake. |
| Fatigue | Persistent exhaustion and lack of energy caused by the inability to utilize glucose effectively. |
| Blurred vision | Distorted or unclear vision resulting from fluid shifts affecting the eye’s lens. |
| Slow healing of wounds | Prolonged healing times for cuts and injuries due to impaired blood flow and immune response. |
| Tingling, pain, or numbness | Abnormal sensations in hands and feet caused by diabetic neuropathy. |
| Dry, itchy skin | Skin issues stemming from dehydration and impaired healing. |
| Increased risk of infections | Higher susceptibility to urinary tract infections, skin infections, and respiratory infections. |
Conclusion
Recognizing the symptoms of diabetes is of utmost importance for early diagnosis and effective management of the condition. Awareness of these symptoms can empower individuals to take proactive steps towards monitoring their health and seeking medical attention when necessary. Timely intervention can significantly improve the prognosis and quality of life for those affected by diabetes, reducing the risk of long-term complications.
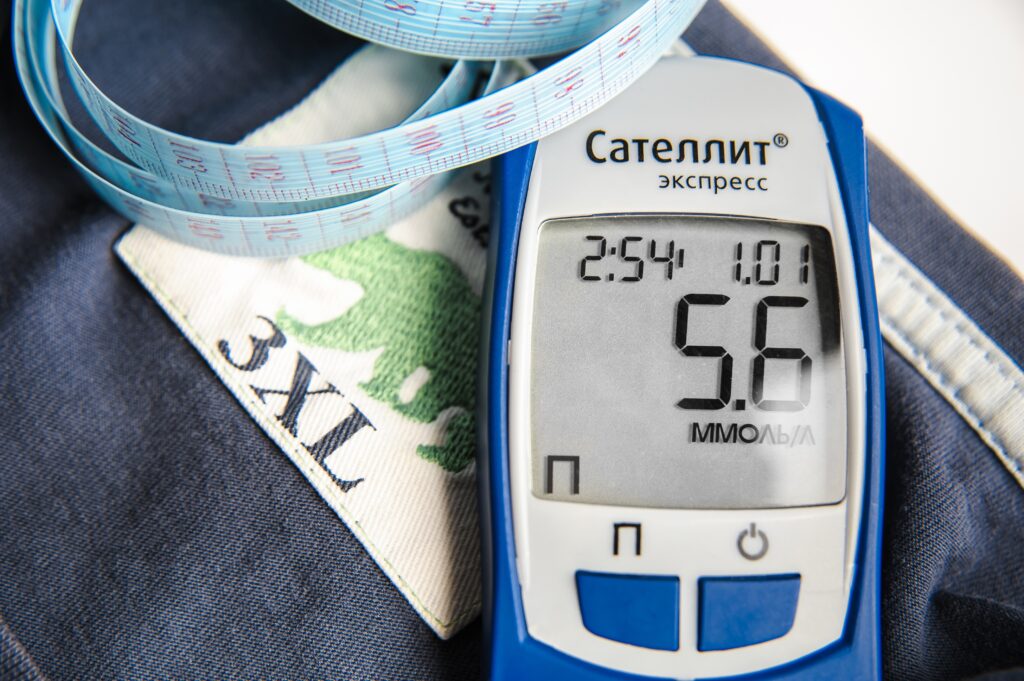
Prevention strategies, including maintaining a healthy lifestyle, managing weight, eating a balanced diet, and engaging in regular physical activity, are essential for minimizing the risk of developing diabetes. Those already diagnosed should prioritize regular check-ups, consistent monitoring of blood sugar levels, and adherence to prescribed treatment plans to maintain optimal health.
By fostering a comprehensive understanding of diabetes and its associated symptoms, we can work together to promote awareness, advocate for healthier lifestyles, and ultimately improve the well-being of individuals living with this chronic condition.
Additional Information on Diabetes Symptoms
| Symptom | Potential Complications |
|---|---|
| Frequent urination (polyuria) | Increased risk of dehydration and urinary tract infections. |
| Increased thirst (polydipsia) | Potential for electrolyte imbalances and kidney stress. |
| Unexplained weight loss | Muscle loss and malnutrition, leading to overall weakness. |
| Extreme hunger (polyphagia) | Risk of overeating and potential weight gain. |
| Fatigue | Impaired concentration and reduced quality of life. |
| Blurred vision | Increased risk of diabetic retinopathy and vision loss. |
| Slow healing of wounds | Risk of infections and complications leading to amputations. |
| Tingling, pain, or numbness | Progressive nerve damage leading to severe complications. |
| Dry, itchy skin | Increased risk of skin infections and irritations. |